Understanding Anal Fistula: Symptoms & Treatment
Explore the symptoms, causes, and effective treatment options for anal fistula. Learn about the signs to watch for and the best approaches to manage this condition.
Symptoms of Anal Fistula
The symptoms of an anal fistula can vary widely among individuals, yet several common signs often indicate the presence of this condition. One of the primary symptoms is discomfort or pain during bowel movements. This pain may become more pronounced after a procedure or an infection, making daily activities a challenge for many afflicted. Individuals may also experience swelling around the anus, which can be a source of discomfort and further complicate hygiene practices.
Additionally, the presence of pus or blood is a significant symptom of an anal fistula. Patients may notice discharge that can be foul-smelling, particularly if an infection is present. Such symptoms can sometimes lead to confusion, as they might resemble those linked to hemorrhoids or other rectal conditions. Thus, it is essential to have a thorough evaluation to arrive at an accurate diagnosis.
Furthermore, symptoms may evolve based on the severity and stage of the fistula. In the early stages, a person might experience minimal discomfort and infrequent discharge, but as the condition progresses, the signs may intensify. For instance, chronic pain, increased frequency of discharge, and more significant inflammation around the anal region can occur. Individuals should be vigilant for warning signs, such as a persistent change in bowel habits, worsening pain, or frequent episodes of infection, prompting them to seek medical assistance.
It is essential to recognize that early diagnosis and management can help prevent complications that may arise from untreated anal fistulas. Comprehensive awareness of the symptoms associated with this condition empowers patients to advocate for their health and seek appropriate treatment when necessary.
Causes of Anal Fistula
Anal fistulas often result from a variety of underlying conditions that affect the anal area. One significant factor contributing to the formation of anal fistulas is inflammatory bowel disease (IBD), which includes conditions such as Crohn's disease and ulcerative colitis. These chronic conditions can lead to inflammation of the intestinal tract, often resulting in abscesses, which are localized infections that can subsequently develop into fistulas if not properly treated.
Infections also play a critical role in the development of anal fistulas. For instance, an anal abscess, which is a painful collection of pus near the anus, can occur due to bacterial infections, and if the abscess is not drained effectively, it may create a channel or tunnel to the skin, forming a fistula. Furthermore, trauma to the anal area, such as during childbirth or surgical procedures, may damage the surrounding tissue, predisposing individuals to the formation of anal fistulas.
Previous surgical complications can lead to fistulas as well. Surgical interventions that involve the rectum or anals can sometimes result in unintended injury to surrounding structures, which may ultimately result in the development of a fistula. Additionally, sexually transmitted infections (STIs), such as HIV or gonorrhea, can also result in fistula formation, particularly in individuals whose immune systems may already be compromised. Less commonly, malignancies in or around the anal region can result in fistulas, often indicating a more serious underlying issue that requires immediate medical attention.
In summary, the causes of anal fistulas are diverse and multifactorial, ranging from chronic inflammatory conditions to surgical complications and infections. Understanding these causes is essential for effective diagnosis and treatment of anal fistulas, as addressing the underlying factors can significantly improve outcomes for patients.
Diagnosis of Anal Fistula
The diagnosis of an anal fistula is a multifaceted process that primarily begins with a comprehensive clinical assessment conducted by healthcare professionals. This initial evaluation emphasizes the importance of gathering a detailed medical history. Patients are typically asked about their symptoms, duration, and previous medical conditions, as well as any history of anal or rectal surgery, inflammatory bowel diseases, or infections. This background allows the physician to identify potential underlying causes that may contribute to the formation of an anal fistula.
A thorough physical examination is paramount in the diagnostic process. During this examination, the healthcare provider inspects the anal region for any visible signs of a fistula, such as swelling, redness, or discharge. This visual inspection may be complemented by a digital examination, wherein the physician uses a gloved finger to assess the surrounding tissue and identify any palpable abnormalities. Such examinations often reveal critical information regarding the nature of the fistula, including its location and potential complications.
In some cases, advanced imaging techniques may be necessary to obtain a clearer understanding of the fistula's extent and characteristics. Magnetic Resonance Imaging (MRI) and endoscopic evaluations are two sophisticated options employed in these situations. MRI is especially useful for delineating the anatomy of the anal canal and assessing the presence of any associated abscesses or sinus tracts. Endoscopy, on the other hand, provides a visual representation of the internal structures, allowing the physician to ascertain the precise type and severity of the fistula.
Recognizing the significance of identifying underlying conditions is crucial, as certain diseases, such as Crohn's disease or tuberculosis, can significantly influence the management and prognosis of an anal fistula. A well-rounded diagnostic approach not only aids in determining effective treatment options but also helps mitigate the risk of recurrence, thereby promoting long-term patient well-being.
Treatment Options for Anal Fistula
When addressing anal fistulas, it is essential to consider a variety of treatment options tailored to the individual’s condition and overall health status. Treatment can range from conservative management to surgical interventions, depending on the complexity of the fistula and the severity of symptoms. Initial non-invasive approaches may include the use of antibiotics to treat any concurrent infection and sitz baths to relieve discomfort. While these methods can provide temporary symptom relief, they do not resolve the fistula itself and are generally regarded as adjuncts to more definitive treatments.
Surgical intervention is often necessary for a complete resolution of an anal fistula. One common procedure is fistulotomy, where the fistula tract is opened and laid flat to allow for healing from within. This technique is particularly effective for simple fistulas, offering a high success rate; however, it may not be suitable for more complex or recurrent cases.
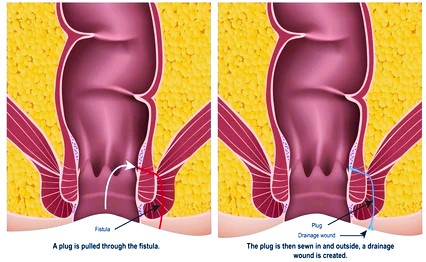
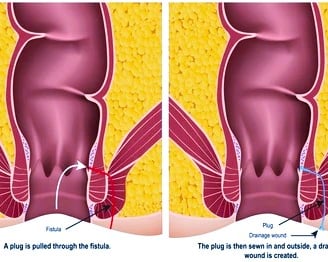
Another surgical option is seton placement. This involves inserting a piece of surgical thread through the fistula to promote drainage and gradual cutting of the tissue over time. Setons are particularly useful for managing high or complex anal fistulas and can reduce the risk of complications while encouraging healing.
For patients with more intricate fistula configurations, advancement flaps may be utilized. This technique involves covering the fistula opening with a flap of healthy tissue, promoting healing while minimizing the risk of recurrence. Each of these surgical options carries potential risks, including pain, infection, and in some cases, complications such as incontinence.
Post-treatment care is crucial in promoting recovery and mitigating the chances of recurrent fistulas. Following surgical intervention, patients are typically advised to maintain proper hygiene, track any symptoms of infection, and engage in follow-up appointments to monitor healing. Understanding each treatment option's indications and possible outcomes enables patients to make informed decisions regarding their anal fistula management strategy.
