Melena: Causes & Treatments for Black Stool
Discover the causes of melena and learn about effective treatments for black stool. Understand the symptoms and when to seek medical attention for this condition.
What is Melena?
Melena refers to the passage of black, tarry stools, which is often indicative of upper gastrointestinal bleeding. This condition distinguishes itself from other forms of stool discoloration, such as those caused by dietary choices or certain medications. The dark coloration of melena is primarily due to the oxidation of iron in the hemoglobin of blood, a process that occurs as the blood moves through the gastrointestinal tract. This oxidation, coupled with the bacterial breakdown of blood, gives melena its characteristic tar-like appearance, making it a significant medical symptom that warrants attention.
Typically, melena is associated with bleeding from sources such as the esophagus, stomach, or small intestine. Unlike hematochezia, which presents as bright red blood in the stools and usually signifies lower gastrointestinal bleeding, melena implies that the blood has had time to undergo chemical changes. As such, it usually appears dark and sticky—a stark contrast to fresh blood. Recognizing melena is crucial, as its presence can indicate serious underlying conditions, such as stomach ulcers, varices, or malignancies. The texture of melena often resembles that of tar, a visual cue that should prompt immediate medical evaluation.
It is essential to approach any instance of black stool with caution. While melena is a symptom linked to significant health issues, it may also be influenced by non-pathological factors, such as iron supplements or certain foods. Given its association with upper gastrointestinal bleeding, the manifestation of melena should be considered a medical emergency, necessitating prompt investigation to establish the source of bleeding and initiate appropriate treatment. Ignoring these symptoms can lead to detrimental health consequences, underscoring the importance of understanding melena and its implications within the broader context of gastrointestinal health.
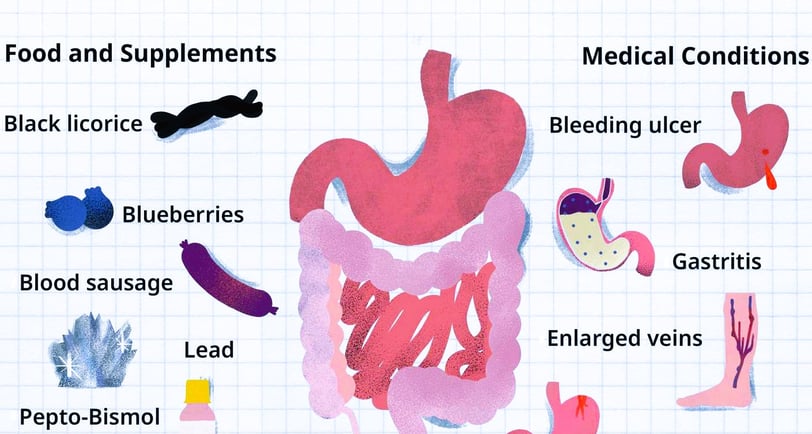
Common Causes of Melena
Melena, characterized by black, tarry stools, is often indicative of underlying gastrointestinal bleeding. The identification of the specific causes is crucial for effective management and treatment. This condition can arise from several key categories, particularly gastrointestinal bleeding, ulcers, liver disease, medication use, and dietary factors.
One of the primary causes of melena is gastrointestinal bleeding, which can originate from various sources in the digestive tract. This could include the esophagus, stomach, or the upper part of the small intestine. Conditions such as peptic ulcers are a prevalent source of bleeding; these can become exacerbated by factors such as long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), which can lead to mucosal damage and subsequent bleeding.
Another important group of causes includes liver disease, particularly cirrhosis, which can result in the development of esophageal varices—dilated veins that can rupture and cause significant bleeding. This bleeding may manifest as melena, alerting individuals of a potential health crisis that requires immediate attention.
Additionally, certain medications and dietary factors can contribute to melena. While NSAIDs and corticosteroids are well-known for their association with gastrointestinal bleeding, heavy alcohol consumption and specific foods can also lead to black stools. For example, consuming large amounts of black licorice or iron supplements may color the stool dark without any underlying pathology.
Recognizing the various conditions that lead to melena, such as diverticulosis or malignancies, is essential for early diagnosis and intervention. It is imperative for individuals experiencing melena to seek medical evaluation promptly, as this symptom can be a sign of serious health issues that require immediate care.
Diagnosing Melena
Diagnosing melena begins with a comprehensive approach, often initiated by healthcare providers conducting a thorough medical history review. During this stage, clinicians inquire about the patient’s symptoms, including the onset and characteristics of the black stool, alongside any concurrent symptoms such as abdominal pain, fatigue, or dizziness. This initial discussion is critical, as it helps to identify potential underlying causes of melena and informs subsequent diagnostic steps.
Following the medical history, a physical examination is typically performed. The provider may assess the patient for signs of anemia, such as paleness, and examine the abdomen for any tenderness or distension. These preliminary findings can give clues about the urgency of the situation and whether immediate intervention may be necessary.
If melena is suspected, several diagnostic tests can be employed to further investigate the potential causes. One of the most prominent procedures is endoscopy, which allows direct visualization of the gastrointestinal tract. This technique can help identify lesions, ulcers, or sources of bleeding, dispelling uncertainties regarding the origins of the melena. Additionally, stool tests may be performed to check for the presence of blood or pathogens, providing insights into whether the black stool is a result of gastrointestinal bleeding or other factors such as dietary influences.
Imaging studies, such as abdominal ultrasounds or CT scans, may also be warranted in complex cases. These tests help evaluate the structural aspects of the gastrointestinal system and can reveal issues such as tumors or obstructions, contributing to the overall understanding of the patient's condition. Symptoms that manifest alongside melena, such as vomiting blood or pronounced abdominal distress, may necessitate urgent evaluation to mitigate potential risks. In summary, an accurate diagnosis of melena requires a meticulous approach, combining medical history, physical examination, and targeted diagnostic tests to ensure timely treatment and address any serious underlying conditions.
Treatment Options for Melena
Treatment for melena primarily targets both its symptomatic management and the underlying causes. Given that melena typically indicates gastrointestinal bleeding, the first priority is to stabilize the patient, particularly in severe cases that may necessitate hospitalization. Healthcare providers often initiate treatment with intravenous fluids to maintain hydration and blood volume. Additionally, medications such as proton pump inhibitors may be prescribed to reduce gastric acid secretion, thereby promoting healing and controlling further bleeding.
In cases where bleeding is significant, more aggressive interventions may be required. Endoscopy plays a crucial role in treatment; either an upper endoscopy or colonoscopy can be employed to locate the source of bleeding and enable therapeutic measures, such as cauterization or band ligation to stop the hemorrhage. Surgical interventions might also be necessary for severe or persistent cases wherein other treatments have failed, particularly if structural abnormalities or tumors are identified as the underlying causes.
Alongside these medical interventions, lifestyle modifications are essential for effective management and the prevention of recurrence. A diet rich in fiber can aid in digestive health and may provide some protection against gastrointestinal issues. Avoiding irritants such as alcohol and non-steroidal anti-inflammatory drugs (NSAIDs) is also recommended, as these can exacerbate gastrointestinal bleeding. Regular follow-up care is vital to ensure that the treatment is effective and to monitor for any signs of recurrence. Patients should be advised to seek immediate medical attention if they experience any worsening symptoms, such as increased black stool volume, dizziness, or significant abdominal pain, as these may indicate a serious underlying issue.
