Understanding Bone Mineral Density Tests
Learn everything you need to know about bone mineral density tests, their importance for bone health, and how to interpret your results. Ensure your bone density is optimal for a healthier lifestyle.
What is a Bone Mineral Density Test?
A Bone Mineral Density (BMD) test is a medical assessment designed to measure the amount of mineral content in bones, primarily calcium and phosphorus. This test is crucial for evaluating bone health and strength, significantly contributing to the diagnosis and management of osteoporosis and other bone-related conditions. By quantifying mineral density, healthcare professionals can ascertain the risk of fractures and other complications associated with weakened bones.
The underlying principle of BMD testing involves the use of specialized imaging techniques, most commonly dual-energy X-ray absorptiometry (DEXA). This non-invasive method allows for precise measurement of bone mineral density at various skeletal sites, making it an essential tool for assessing overall skeletal health. During the test, low-dose X-ray beams differentiate between bone and soft tissue to provide accurate readings of bone density. The results are then compared to standardized values in a healthy population, allowing healthcare providers to identify areas of concern.
Bone mineral density tests play a vital role in the early detection of osteoporosis, a condition characterized by low bone density that increases the likelihood of fractures. Additionally, BMD testing is beneficial in monitoring individuals with existing conditions that might affect bone health, such as hormonal imbalances or prolonged use of certain medications. Healthcare professionals typically look for specific values in the results, including T-scores and Z-scores, which indicate how an individual’s bone density compares to healthy younger adults and individuals of the same age and sex, respectively. Overall, the BMD test is a crucial element in preventive healthcare, facilitating timely interventions to preserve bone integrity and reduce the risk of fractures.
Who Should Get a Bone Mineral Density Test?
Bone mineral density (BMD) testing is an important diagnostic tool used to assess the strength and health of bones, particularly as individuals age or when certain risk factors are present. According to various health organizations, specific demographics and health conditions warrant a BMD test to help in the early detection of osteoporosis and related bone disorders.
One of the primary demographics that should consider undergoing a BMD test is individuals aged 65 and older. Women are especially encouraged to get tested post-menopause, as hormonal changes can lead to significant decreases in bone density. Meanwhile, men who are 70 years or older should also prioritize a BMD assessment. Additionally, younger individuals—particularly women under 65 and men under 70—may need screening if they possess risk factors such as a family history of osteoporosis, a previous fracture from low-impact injuries, or specific medical conditions like rheumatoid arthritis, hyperthyroidism, or prolonged use of corticosteroids.
Lifestyle choices also play a significant role in determining the necessity of a BMD test. Individuals who smoke, have excessive alcohol intake, or follow a sedentary lifestyle should consider screening. Furthermore, those who have low body weight or suffer from eating disorders, such as anorexia, are at a greater risk of developing low bone density and may benefit from a BMD test.
Most health organizations recommend that screening should not only be based on age or risk factors but could also be reassessed at regular intervals. For women, tests may be spaced every 2 years, while men may follow similar recommendations based on their health profiles. Overall, consulting with a healthcare provider for personalized advice regarding the timing and frequency of bone mineral density testing is essential.
How is a Bone Mineral Density Test Performed?
A Bone Mineral Density (BMD) test is a vital procedure used to evaluate bone health and assess the risk of osteoporosis and fractures. The most common method for performing this test is called dual-energy X-ray absorptiometry (DEXA). This test involves the use of low-energy X-rays to measure the amount of mineral present in the bone, specifically in the hip and spine, which are critical areas prone to fractures. The DEXA scan is a straightforward, quick process, typically taking around 10 to 30 minutes to complete.
Patients undergoing a DEXA scan are usually advised to wear comfortable, loose-fitting clothing devoid of metal zippers or buttons. Before the procedure, individuals should inform their healthcare provider of any recent scans or medical treatments involving radiation to avoid potential duplication. In some cases, patients may need to refrain from calcium supplements for 24 hours prior to the test to ensure accuracy in results.
Another method utilized for evaluating bone density is quantitative computed tomography (QCT). This advanced imaging technique allows for a three-dimensional analysis of bone density, offering a more detailed assessment compared to DEXA. However, QCT is less commonly used due to its higher cost and increased radiation exposure. Patients who undergo QCT should expect a longer testing time and may be required to lie still on a table while the scanner moves around them.
Concerns regarding the safety and accuracy of BMD tests, particularly regarding radiation exposure, are common among patients. It is important to note that the amount of radiation used in DEXA scans is minimal, significantly less than that of a standard X-ray. These tests provide crucial insights into bone health, enabling early detection of conditions that could lead to fractures. Therefore, the benefits of undergoing a BMD test generally outweigh potential risks associated with radiation exposure.
Understanding Your Bone Mineral Density Test Results
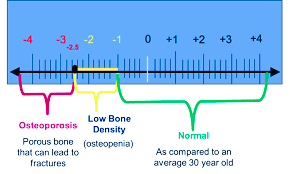
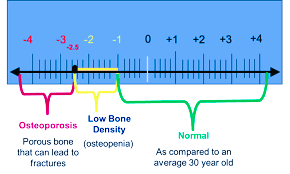
Interpreting your bone mineral density (BMD) test results is crucial for understanding your bone health. A primary element of these results is the T-score, which compares your bone density to that of a healthy young adult of the same gender. It indicates whether your bone density is normal, low, or indicative of osteoporosis. A T-score of -1.0 or above is considered normal. Scores between -1.0 and -2.5 suggest low bone density, also termed osteopenia, while scores of -2.5 or lower indicate osteoporosis. These classifications are vital, as they guide clinical decision-making regarding the need for treatment.
Alongside the T-score, the Z-score is also important, which compares your bone density with that of individuals of the same age and gender. The Z-score helps contextualize your results in relation to your unique demographics. A Z-score above -2.0 is generally seen as normal, while a score below this threshold may prompt further investigation into possible underlying causes of bone loss.
Upon reviewing your BMD results, it's essential to discuss potential next steps with your healthcare provider. Depending on the T-score and Z-score, lifestyle changes may be recommended, which include increasing dietary calcium and vitamin D intake, incorporating weight-bearing exercises, and avoiding smoking and excessive alcohol consumption. If your results indicate significant bone density loss, medication options may also be explored to help strengthen your bones.
Moreover, regular follow-ups and potential additional testing are crucial for monitoring bone health. These check-ups ensure that any changes in your bone density are tracked over time, enabling timely interventions if necessary. Prioritizing your bone health through understanding and acting on BMD test results is a key component of maintaining overall well-being.
