Fatty Liver: Causes, Symptoms & Treatment
Explore the causes, symptoms, and effective treatment options for fatty liver disease. Learn how to manage and improve your liver health with practical advice and insights.
What is Fatty Liver?
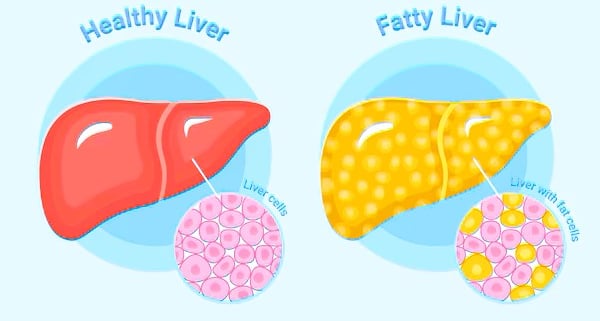
Fatty liver disease is a condition characterized by the abnormal accumulation of fat within liver cells. This excess fat can disrupt normal liver function and may lead to a range of health complications if left untreated. The condition is generally classified into two primary categories: alcoholic fatty liver disease (ALD) and non-alcoholic fatty liver disease (NAFLD). ALD occurs as a result of excessive alcohol consumption, leading to liver inflammation and, over time, potential liver damage. In contrast, NAFLD is not related to alcohol intake and is frequently associated with obesity, type 2 diabetes, and metabolic syndrome.
The accumulation of fat in the liver can result from several factors, primarily involving disruptions in fat metabolism. When the body metabolizes fats, it either utilizes them for energy or stores them in adipose tissues. However, when there is an imbalance—such as increased fat production, reduced fat export from the liver, or a lack of fat breakdown—fat begins to accumulate within liver cells. This excess fat can interfere with the liver's ability to govern vital metabolic processes, eventually leading to inflammation, fibrosis, or even cirrhosis in severe cases.
Fatty liver disease is often asymptomatic in its early stages, making it challenging to diagnose without imaging tests or blood work. However, as the condition progresses, individuals may experience symptoms such as fatigue, weight loss, and discomfort in the upper right abdomen. Given the implications of fatty liver on overall health, it is crucial to recognize the risk factors—such as poor diet, sedentary lifestyle, and genetic predisposition—and to implement lifestyle changes that can mitigate the progression of this condition. Effective management is vital for maintaining liver health and overall well-being.
Causes of Fatty Liver
Fatty liver disease, or hepatic steatosis, is a condition characterized by the accumulation of excess fat in liver cells. Understanding the multifaceted causes of fatty liver is crucial for effective prevention and management. One of the leading contributors to this ailment is obesity. Excess body weight, particularly around the abdomen, increases the likelihood of fat deposition in the liver. As obesity rates continue to rise globally, so does the prevalence of fatty liver disease.
Another significant factor is diabetes, especially Type 2 diabetes. High blood sugar levels can lead to excessive fat storage in the liver, exacerbating the condition. The metabolic disruptions associated with diabetes, including insulin resistance, are major catalysts for fatty liver development. Similarly, high cholesterol levels and triglycerides contribute to altered lipid metabolism, further increasing the risk of fatty liver disease.
Excessive alcohol consumption is another well-documented cause of fatty liver. Chronic alcoholism can result in alcohol-induced liver injury, leading to fat buildup. However, not all individuals with fatty liver consume large amounts of alcohol, illustrating the condition's complexity. In fact, some cases occur in individuals who follow a healthy lifestyle, highlighting the role of genetics and other non-modifiable factors.
A sedentary lifestyle has also been linked to the development of fatty liver disease. Regular physical activity is essential for maintaining healthy liver function, as exercise aids in the metabolism of fats and sugars. Furthermore, poor dietary habits, characterized by high sugar and fat intake, exacerbate the risk for fatty liver disease, demonstrating the interplay between diet and lifestyle choices.
Understanding these causes aids in recognizing the importance of lifestyle modifications and medical interventions that can mitigate the risks associated with fatty liver disease.
Symptoms of Fatty Liver
Fatty liver disease, which manifests when excess fat accumulates in liver cells, is often asymptomatic in its early stages. However, as the condition progresses, various symptoms may emerge that indicate the liver is struggling to function effectively. Recognizing these warning signs is crucial for timely medical intervention and effective management of the disease.
One of the most common initial symptoms is persistent fatigue. Individuals may feel unusually tired or weak, even with adequate rest. This fatigue can stem from the liver's compromised ability to process nutrients and detoxify the body. Along with fatigue, many people with fatty liver report discomfort or pain in the upper abdomen, particularly in the right upper quadrant, where the liver is located. This discomfort can manifest as a dull ache or a feeling of fullness in the abdomen.
As fatty liver disease progresses, additional symptoms may arise. Weight loss without trying is a significant warning sign, often accompanied by a loss of appetite. Some individuals may experience nausea, which can further contribute to dietary issues and malnutrition. Furthermore, skin changes can occur, such as easy bruising or yellowing of the skin and eyes (jaundice), indicating that the liver is unable to adequately filter toxins and waste products from the bloodstream.
In some cases, swelling in the abdomen or legs may occur due to fluid accumulation, a condition known as ascites. This swelling can lead to discomfort and hinder daily activities. It is essential to pay attention to these symptoms and consult a healthcare professional if they present, as early detection and management can significantly improve outcomes in individuals with fatty liver disease.
Diagnosis of Fatty Liver
Diagnosing fatty liver disease involves a combination of medical history evaluation, physical examination, and various diagnostic tools. Healthcare professionals often begin by assessing the patient's risk factors, which include obesity, diabetes, and high cholesterol. After this preliminary assessment, several methods may be employed to confirm the presence of fatty liver and determine its severity.
One of the initial diagnostic tools used is blood tests. Liver function tests (LFTs) can provide valuable information regarding the health of the liver. Elevated liver enzymes, such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST), may suggest liver inflammation or damage, indicative of fatty liver disease. Additionally, tests to evaluate metabolic factors and screen for viral hepatitis may be conducted to rule out other liver-related concerns.
Imaging techniques play a vital role in diagnosing fatty liver disease. Ultrasound is commonly used as a non-invasive first-line imaging modality. This technique can detect fat deposits within the liver and assess its size and appearance. However, if further clarification is required, advanced imaging methods such as computed tomography (CT) scans or magnetic resonance imaging (MRI) may be utilized. These imaging tests provide more detailed views and can help quantify the extent of fat accumulation.
In certain cases, a liver biopsy may be performed to obtain definitive diagnosis and assess the degree of liver injury. During this procedure, a small sample of liver tissue is extracted and analyzed for fat content, inflammation, and fibrosis. This method is particularly useful when the diagnosis remains uncertain after non-invasive imaging and laboratory tests or when there is a need to evaluate the degree of liver damage.
Ultimately, accurate diagnosis is essential for proper management and treatment of fatty liver disease, guiding healthcare providers in developing personalized care plans for patients.
Treatment Options for Fatty Liver
Fatty liver disease, characterized by an excess accumulation of fat in liver cells, can be managed through a variety of treatment options. The first line of defense typically involves lifestyle modifications, which play a crucial role in managing the condition. These changes may include increasing physical activity, reducing caloric intake, and adopting a healthier diet. Diets rich in fruits, vegetables, whole grains, and lean proteins can ameliorate the effects of fatty liver.
Weight loss stands out as a significant factor in reversing fatty liver disease. A reduction of just 5% to 10% of body weight has been associated with improved liver health. This can often be achieved through a combination of regular exercise and caloric restriction. The importance of maintaining a balanced diet cannot be understated; reducing sugar intake, particularly from sugary beverages and snacks, as well as moderating fat consumption, helps in managing the disease effectively.
In addition to lifestyle changes, dietary management is crucial. The Mediterranean diet, known for its emphasis on healthy fats like olive oil, along with lean protein sources such as fish and legumes, has shown promise in promoting liver health. Moreover, ensuring adequate hydration and limiting alcohol consumption are essential components of dietary strategies for managing fatty liver.
For individuals with more severe cases of fatty liver, medical treatments may be necessary. While specific medications are still under research, some current options include insulin sensitizers and vitamin E supplementation. In extreme cases where liver function continues to deteriorate, surgical interventions, such as liver transplant, may be considered. Overall, an individualized approach that incorporates lifestyle changes, dietary modifications, weight management, and medical treatments is essential for effectively managing fatty liver disease.
Preventing Fatty Liver Disease
Preventing fatty liver disease is fundamentally intertwined with the adoption of a healthy lifestyle that prioritizes balanced nutrition and regular physical activity. A well-rounded diet plays a crucial role in liver health, emphasizing the need for whole foods rich in nutrients. Incorporating fruits, vegetables, whole grains, lean proteins, and healthy fats can help maintain a healthy body weight, which is vital in preventing the accumulation of fat in the liver. Limiting processed foods, refined sugars, and saturated fats can also significantly reduce the risk of developing fatty liver disease.
Maintaining a healthy weight is vital for liver health, as obesity is one of the primary risk factors associated with fatty liver disease. Regular physical activity, ideally at least 150 minutes of moderate aerobic exercise each week, can significantly aid in weight management. Incorporating strength training exercises at least two days a week will further enhance metabolic health and contribute to the prevention of fatty liver disease. It is essential to find physical activities that are enjoyable to ensure consistency in exercise routines.
In addition to diet and exercise, regular medical check-ups are paramount in the prevention of fatty liver disease. Health professionals can provide essential screenings and risk assessments, which can help in early detection of liver issues. Monitoring blood sugar levels, cholesterol levels, and liver enzyme counts can offer insights into one’s liver health status. For individuals at higher risk, such as those with diabetes or metabolic syndrome, seeking guidance from healthcare providers on personalized prevention strategies is advisable.
Implementing these lifestyle changes not only bolsters liver health but also promotes overall wellbeing. Through informed dietary choices, consistent physical activity, and proactive health monitoring, individuals can take crucial steps towards preventing fatty liver disease and safeguarding their liver functionality for the future.
Living with Fatty Liver: Patient Stories and Support
Individuals grappling with fatty liver disease often encounter a myriad of emotional and physical challenges that significantly impact their daily lives. Stories from patients reveal a spectrum of experiences, underscoring the complexities of managing this condition. For many, the diagnosis comes as a shock, leading to a profound sense of uncertainty regarding their health and future. One patient might describe the frustration of adhering to a stringent diet while watching friends enjoy indulgent meals. Others may express feelings of isolation, as fatty liver disease is not always visible to those outside their immediate circle, which can lead to a lack of understanding from family and friends.
The emotional toll of living with fatty liver disease often intertwines with the physical symptoms. Fatigue, discomfort, and anxiety about long-term health effects can create a challenging environment for patients. For instance, a 45-year-old man might reflect on how his energy levels have plummeted since his diagnosis, hindering both his professional life and personal pursuits. These shared narratives emphasize the necessity of a supportive network, showcasing how patient storytelling can foster empathy and connection.
Fortunately, support is readily available for those coping with the ramifications of fatty liver disease. Support groups, both in-person and online, provide communities for sharing experiences and practical advice. Websites dedicated to liver health often host forums where patients can converse anonymously about their challenges and triumphs. Resources such as educational webinars, nutritional workshops, and counseling services play an integral role in equipping patients and their families with the tools needed for better management of this condition. Engagement in such communities fosters a sense of hope and belonging, ultimately transforming individual stories into collective advocacy for improved understanding and treatment of fatty liver disease.
