Female Reproductive System and Health Management
Learn about the female reproductive system and how to properly manage reproductive health in women. Explore tips and guidance for optimal women's health. #female reproductive system
Understanding the Female Reproductive System
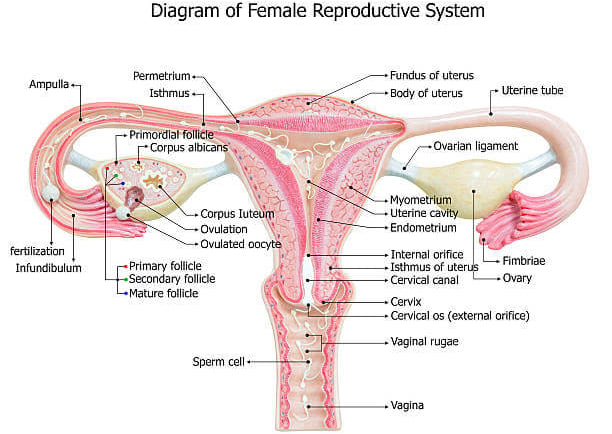
The female reproductive system is an intricate network of organs and structures designed to perform a series of complex and vital functions. Central to this system are the ovaries, fallopian tubes, uterus, and vagina, each playing a distinct role in reproductive health and processes.
The ovaries, located on either side of the uterus, are responsible for producing eggs (ova) and secreting hormones such as estrogen and progesterone. These hormones are crucial in regulating the menstrual cycle and maintaining pregnancy. During ovulation, an ovary releases a mature egg into the fallopian tube.
The fallopian tubes serve as passageways for the eggs to travel from the ovaries to the uterus. Fertilization typically occurs within these tubes if sperm is present, leading to the formation of a zygote.
The uterus, a pear-shaped muscular organ, provides a nurturing environment for a fertilized egg to implant and develop into a fetus. The lining of the uterus, known as the endometrium, thickens each month in preparation for potential pregnancy. If fertilization does not occur, the endometrial lining sheds during menstruation.
The vagina functions as the canal that connects the external genitals to the uterus. It serves multiple roles, including the passage of menstrual flow, the receptacle for sperm during intercourse, and the birth canal during delivery.
Hormonal regulation is a pivotal aspect of the female reproductive system. Estrogen and progesterone are the primary hormones involved, orchestrating the menstrual cycle and preparing the reproductive organs for potential pregnancy. Estrogen is mainly responsible for the development of secondary sexual characteristics and the regulation of the menstrual cycle, while progesterone prepares the endometrium for implantation and supports early pregnancy.
Understanding the female reproductive system's anatomy and hormonal regulation is fundamental to grasping how processes such as menstruation, ovulation, and pregnancy occur. This knowledge is essential for managing reproductive health and addressing any potential issues that may arise.
Common Reproductive Health Issues
The female reproductive system is complex and can be affected by various health issues that may impact overall well-being and fertility. Understanding these common conditions, their symptoms, causes, and treatment options is crucial for proper management and seeking timely medical advice.
Menstrual Disorders: Menstrual disorders encompass a range of conditions including dysmenorrhea and amenorrhea. Dysmenorrhea refers to painful menstrual cramps that can interfere with daily activities. Primary dysmenorrhea is often caused by the release of prostaglandins, while secondary dysmenorrhea might be linked to conditions like endometriosis or fibroids. Amenorrhea is the absence of menstrual periods, which could be primary (no menstruation by age 15) or secondary (stopping of menstruation for three months or more). Causes range from hormonal imbalances to excessive exercise or significant weight loss. Treatments may include pain relievers, hormonal therapies, and lifestyle modifications.
Polycystic Ovary Syndrome (PCOS): PCOS is characterized by enlarged ovaries containing small cysts. Symptoms include irregular periods, excessive hair growth, acne, and obesity. The exact cause is unknown, but insulin resistance and hormonal imbalances play significant roles. PCOS can affect fertility due to irregular ovulation. Treatments aim at managing symptoms and may include lifestyle changes, medications to regulate menstrual cycles, and fertility treatments.
Endometriosis: Endometriosis occurs when tissue similar to the lining inside the uterus starts growing outside it, often causing severe pain, especially during menstruation. It can also lead to fertility issues. The cause remains unclear, but retrograde menstruation and immune system disorders are potential factors. Treatment options include pain relief medications, hormonal therapies, and surgical interventions to remove excess tissue.
Fibroids: Uterine fibroids are benign tumors that develop in the uterus, commonly during childbearing years. They can cause heavy menstrual bleeding, pelvic pain, and pressure symptoms. The exact cause is unknown, but hormonal and genetic factors may contribute. Treatment varies based on the severity and includes medications to manage symptoms, non-invasive procedures, and surgical options like myomectomy or hysterectomy.
These conditions can significantly impact reproductive health and fertility, making it essential to seek medical advice when symptoms arise. Gynecologists and reproductive endocrinologists are specialized healthcare professionals who can provide appropriate diagnosis and treatment plans, ensuring comprehensive care for women's reproductive health.
Proper Management and Care Tips
Maintaining a healthy female reproductive system is crucial for overall well-being. Regular gynecological check-ups are essential, as they help in early detection of potential issues and ensure that you are up-to-date with necessary screenings, such as Pap smears and mammograms. These visits also provide an opportunity to discuss any concerns related to menstrual health, sexual health, or other reproductive issues.
Adopting a healthy lifestyle is another cornerstone of reproductive health. A balanced diet rich in fruits, vegetables, whole grains, and lean proteins supports hormonal balance and overall function of the reproductive system. Regular exercise not only helps in maintaining a healthy weight but also reduces the risk of conditions such as polycystic ovary syndrome (PCOS) and enhances mood, which is vital for mental health.
Mental health plays a significant role in reproductive health. Stress management techniques, such as mindfulness, meditation, or yoga, can alleviate symptoms of premenstrual syndrome (PMS) and contribute to a balanced hormonal environment. Ensuring adequate sleep and seeking support for mental health issues like anxiety or depression can also be beneficial.
Menstrual health management is crucial. Using appropriate menstrual products, whether they are pads, tampons, or menstrual cups, and maintaining proper hygiene can prevent infections and discomfort. It’s also important to track your menstrual cycle to identify any irregularities that may need medical attention.
Safe sexual practices and contraception options should not be overlooked. Using condoms can prevent sexually transmitted infections (STIs), while discussing other forms of contraception with your healthcare provider can help in choosing the right method for your needs.
Self-examinations and being aware of changes in your body can help in catching potential issues early. Regular breast self-exams and being vigilant about any unusual symptoms or changes in your reproductive system are important preventive measures.
Navigating reproductive health during different life stages requires specific attention. During puberty, proper education on menstrual health and safe sexual practices is essential. In adulthood, regular screenings and maintaining a healthy lifestyle are key. As you approach menopause, understanding the changes in your body and seeking appropriate care can ease the transition.
