Hepatitis C: Causes, Symptoms, Diagnosis & Treatment Options
Learn about Hepatitis C causes, transmission, symptoms, diagnosis, and modern treatment options to prevent liver damage and long-term complications. #Hepatitis C #virus

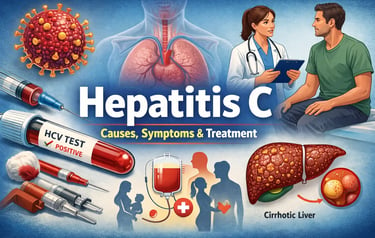
Causes, Transmission, Symptoms, Diagnosis, and Treatment of Hepatitis C
Causes and Transmission of Hepatitis C
Hepatitis C is a viral infection caused by the Hepatitis C virus (HCV) that primarily affects the liver. The virus is mainly transmitted through blood-to-blood contact, making certain behaviors and exposures high risk for infection.
One of the most common causes of Hepatitis C transmission is the sharing of needles, syringes, or other injecting equipment, especially among people who use intravenous drugs. Even microscopic amounts of infected blood on needles or tools can spread the virus. Another significant risk factor is the use of unsterilized or improperly sterilized medical equipment, which may occur in regions with limited healthcare infrastructure or inadequate infection-control practices.
In the past, blood transfusions and organ transplants were a major source of Hepatitis C infection. However, since the introduction of strict blood screening protocols in many countries after 1992, this mode of transmission has become extremely rare. Despite this progress, individuals who received blood products before the implementation of these screening measures remain at higher risk.
Mother-to-child transmission, also known as perinatal transmission, can occur during childbirth if the mother is infected with HCV. While the risk is relatively low, it is still a recognized route of infection. Hepatitis C can also be transmitted through sexual contact, though this is uncommon compared to other bloodborne infections. The risk increases in individuals with multiple sexual partners, co-infection with HIV, or practices that may cause bleeding.
Understanding high-risk groups is essential for prevention and early detection. These groups include intravenous drug users, healthcare workers exposed to needlestick injuries, individuals who underwent medical procedures with unsafe equipment, and recipients of blood transfusions before 1992.
Symptoms of Hepatitis C
Hepatitis C is often called a “silent disease” because many infected individuals experience no symptoms in the early stages. When symptoms do appear, they are often mild and may be mistaken for other common illnesses.
Early symptoms of Hepatitis C may include:
Persistent fatigue
Jaundice (yellowing of the skin and eyes)
Dark-colored urine
Pale or clay-colored stools
Abdominal discomfort
Nausea or loss of appetite
Joint and muscle pain
Fatigue is the most frequently reported symptom and can significantly affect quality of life.
If the infection progresses from acute Hepatitis C (within the first six months of exposure) to chronic Hepatitis C, more serious complications may develop over time. Chronic infection can quietly damage the liver for years, leading to conditions such as liver fibrosis, cirrhosis, liver failure, or liver cancer. Advanced symptoms may include abdominal swelling, easy bruising or bleeding, itchy skin, confusion, and unexplained weight loss.
Diagnosis of Hepatitis C
Early and accurate diagnosis of Hepatitis C is critical for effective treatment and prevention of long-term liver damage. The diagnostic process usually begins with an HCV antibody test, which detects whether a person has ever been exposed to the virus.
If the antibody test is positive, a follow-up HCV RNA test is performed to confirm an active infection by measuring the amount of virus present in the blood. This test helps determine whether treatment is necessary.
Additional liver function tests (LFTs) are commonly used to evaluate liver health by measuring enzyme levels such as ALT and AST. Elevated levels may indicate liver inflammation or damage. In some cases, imaging studies or non-invasive fibrosis assessments may be used to evaluate the extent of liver scarring.
Regular screening is especially important for individuals in high-risk groups, as early detection greatly improves treatment outcomes.
Treatment Options and Management of Hepatitis C
The treatment of Hepatitis C has advanced dramatically with the introduction of direct-acting antivirals (DAAs). These medications directly target the virus and have revolutionized care by offering cure rates exceeding 95% in most patients.
Modern Hepatitis C treatment typically involves an 8 to 12-week course of oral antiviral medication. Commonly prescribed DAAs include sofosbuvir, ledipasvir, daclatasvir, and other combination therapies. Treatment plans are tailored based on factors such as the HCV genotype, viral load, liver condition, and the presence of co-infections like HIV.
DAAs are generally well tolerated, with mild side effects such as headache, fatigue, and nausea reported in some patients. Individuals with advanced liver disease may require closer monitoring and specialized treatment approaches.
Long-Term Management and Lifestyle Considerations
Managing chronic Hepatitis C extends beyond medication. Lifestyle modifications play a vital role in protecting liver health and preventing disease progression. Complete avoidance of alcohol is strongly recommended, as alcohol accelerates liver damage. A healthy, balanced diet rich in fruits, vegetables, whole grains, and lean proteins supports overall liver function.
Regular medical follow-ups are essential, particularly for patients with liver fibrosis or cirrhosis. Ongoing monitoring may include liver function tests, viral load assessments, and screening for liver cancer. With timely treatment, healthy lifestyle choices, and consistent medical care, most individuals with Hepatitis C can achieve a cure and significantly reduce the risk of long-term complications.
