Pulmonary Edema: Causes, Symptoms & Treatments
Discover the causes, symptoms, and effective treatments for pulmonary edema. Learn how to recognize this condition and find comprehensive care options for better health.
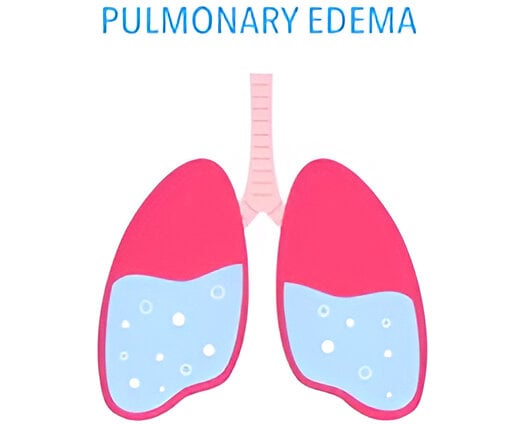
What is Pulmonary Edema?
Pulmonary edema is a medical condition characterized by the abnormal accumulation of excess fluid in the lungs. This condition significantly impacts the body’s ability to exchange oxygen, thereby hindering proper respiratory function. When fluid builds up in the alveoli, which are the tiny air sacs within the lungs, the efficiency of oxygen delivery to the bloodstream is compromised. This can lead to difficulty breathing, a decrease in oxygen levels in the body, and even respiratory failure if not addressed promptly.
The etiology of pulmonary edema can be varied, broadly categorized into cardiogenic and non-cardiogenic types. Cardiogenic pulmonary edema often results from heart-related issues, such as congestive heart failure or myocardial infarction, where the heart's functionality is impaired, leading to increased pressure in the pulmonary blood vessels. On the other hand, non-cardiogenic pulmonary edema may arise due to factors such as infections, exposure to toxins, or acute respiratory distress syndrome (ARDS). These underlying causes can trigger inflammation and capillary leakage, contributing to fluid accumulation.
The seriousness of pulmonary edema cannot be understated, as it poses significant health risks. Symptoms often include shortness of breath, which may worsen with exertion or when lying flat, a feeling of suffocation, and coughing up frothy sputum. These symptoms can create substantial anxiety and discomfort for individuals affected. Furthermore, acute cases can lead to life-threatening complications, necessitating immediate medical intervention to stabilize the patient’s condition and prevent further deterioration. Individuals with pre-existing respiratory or cardiovascular conditions are particularly vulnerable to the adverse effects of pulmonary edema. Understanding this condition is crucial for recognizing its symptoms and seeking timely medical care.
Causes of Pulmonary Edema
Understanding the causes of pulmonary edema is essential for effective diagnosis and treatment. Pulmonary edema can be categorized into two main types: cardiogenic and non-cardiogenic. Each type has distinct underlying issues leading to fluid accumulation in the lungs.
Cardiogenic pulmonary edema is primarily associated with heart-related problems. One of the most common causes is congestive heart failure (CHF), a condition in which the heart is unable to pump blood efficiently. This inefficiency can lead to increased pressure in the heart’s blood vessels, forcing fluids into the lung tissue. Other heart conditions, such as arrhythmias or valvular heart disease, can also contribute to cardiogenic pulmonary edema by similarly affecting the heart’s ability to maintain normal blood circulation.
The non-cardiogenic type, on the other hand, arises from factors unrelated to the heart. Conditions such as pneumonia can cause pulmonary edema due to inflammation and infection in the lungs, prompting fluid to leak into the alveoli. Another cause is exposure to toxins or chemicals, which can irritate lung tissue and lead to permeability changes in the blood vessels. High-altitude pulmonary edema (HAPE) is an additional non-cardiogenic cause, occurring when individuals rapidly ascend to high altitudes, resulting in fluid retention in the lungs exacerbated by hypoxia and increased pulmonary artery pressure.
Risk factors for developing pulmonary edema vary based on the underlying cause. Individuals with pre-existing heart conditions, those with a history of lung infections, or those exposed to high altitudes, pollution, or toxic substances may be at an elevated risk. Awareness of these causes and associated risk factors can aid in recognizing the symptoms early, allowing for timely medical intervention and management of pulmonary edema.
Symptoms of Pulmonary Edema
Pulmonary edema is characterized by an accumulation of fluid in the lungs, leading to various symptoms that can significantly impact an individual’s health. One of the most prominent symptoms is shortness of breath, which may occur suddenly or develop gradually. Patients often describe this feeling as a struggle to catch their breath, especially during physical activity or when lying flat. The severity of this symptom may vary; some individuals may experience mild difficulty, while others swiftly progress to severe respiratory distress.
Coughing is another common symptom associated with pulmonary edema. This may present as a dry cough initially, evolving into a cough that produces frothy sputum, which can be pink or blood-tinged. This change often indicates a worsening state of the condition, warranting immediate medical attention. Additionally, wheezing—a high-pitched, whistling sound produced during breathing—can occur, especially when there is significant obstruction in the airways due to fluid accumulation.
Patients with pulmonary edema may also exhibit signs of increased respiratory rate, referred to as tachypnea. This rapid breathing can be a direct response to insufficient oxygen levels in the bloodstream, prompting the body to work harder to deliver oxygen to tissues. In more severe cases, individuals may show signs of cyanosis, characterized by a bluish tint to the skin, lips, or nails, indicating a critical lack of adequate oxygen. Other associated symptoms can include clammy skin, anxiety, and excessive sweating.
It is important to note that symptoms can vary based on the condition’s severity and how quickly it develops. Recognizing these signs enables individuals to seek timely medical intervention, ultimately improving outcomes in treating pulmonary edema.
Treatment Options for Pulmonary Edema
Pulmonary edema is a serious condition characterized by fluid accumulation in the lungs, which can lead to severe breathing difficulties. Effective treatment strategies are crucial for managing this condition, focusing on both immediate relief and long-term health maintenance. One of the primary treatments for pulmonary edema includes the use of diuretics, which are medications designed to promote the excretion of excess fluid through urine. By reducing fluid overload, diuretics help alleviate the symptoms of pulmonary edema, enabling patients to breathe more easily.
Oxygen therapy is another critical component in the treatment plan for individuals suffering from pulmonary edema. This practice involves administering supplemental oxygen to help increase blood oxygen levels, especially in cases where the fluid accumulation severely impairs gas exchange in the lungs. Individuals with significant respiratory distress may require intubation and mechanical ventilation to ensure adequate oxygen delivery during acute episodes.
Addressing underlying conditions is vital for the effective management of pulmonary edema. For example, patients with heart failure may need specific heart medications, such as ACE inhibitors or beta-blockers, to improve heart function and reduce fluid retention. Moreover, those with renal issues may benefit from interventions aimed at enhancing kidney performance and, consequently, fluid balance in the body.
In addition to these medical treatments, lifestyle modifications can significantly impact long-term outcomes. Patients are often advised to adopt heart-healthy diets low in sodium, engage in regular physical activity, and maintain a healthy weight. Avoiding alcohol and smoking cessation are also essential components of ongoing care to reduce the risk of recurrent episodes. Consequently, a comprehensive treatment approach that combines medications, lifestyle adjustments, and routine follow-up care is imperative for individuals diagnosed with pulmonary edema.
