Sickle Cell Disease: Causes, Symptoms, and Treatment
Learn about the causes, symptoms, and treatment options for sickle cell disease to better understand this condition and how to manage it effectively. #sickle cell anemia
Causes of Sickle Cell Disease
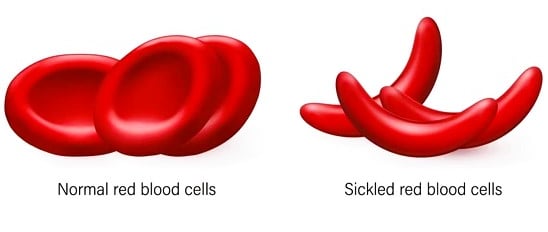
Sickle cell disease is a hereditary disorder caused by a mutation in the hemoglobin subunit beta (HBB) gene. This mutation leads to the production of abnormal hemoglobin, known as hemoglobin S (HbS), which distorts red blood cells into a sickle, or crescent, shape. These abnormally shaped cells are less flexible and can obstruct blood flow, causing various complications.
The inheritance pattern of sickle cell disease is autosomal recessive. This means that for a child to be affected, they must inherit two copies of the mutated HBB gene, one from each parent. Parents who each carry one copy of the mutated gene are considered carriers of the sickle cell trait but typically do not exhibit symptoms of the disease. When both parents are carriers, there is a 25% chance with each pregnancy that their child will inherit both defective genes and develop sickle cell disease.
Sickle cell disease is more prevalent among certain populations, particularly those of African, Mediterranean, Middle Eastern, and Indian ancestry. This higher prevalence is largely due to the evolutionary advantage conferred by the sickle cell trait in regions where malaria is endemic. Carriers of the sickle cell trait, who have one normal hemoglobin gene and one mutated gene, are more resistant to malaria, providing a survival advantage in these regions. Consequently, the sickle cell trait has persisted through generations in areas with high malaria prevalence.
Understanding the genetic basis and inheritance pattern of sickle cell disease is crucial for assessing individual risk and for making informed decisions regarding family planning. Advances in genetic counseling and testing have enabled prospective parents to understand their carrier status and the likelihood of passing the disease to their offspring, thereby facilitating early diagnosis and intervention.
Symptoms and Complications of Sickle Cell Disease
Sickle cell disease (SCD) manifests through a variety of acute and chronic symptoms, resulting from the abnormal, crescent-shaped red blood cells that characterize the condition. These irregular cells impede normal blood flow, leading to a cascade of clinical complications.
One of the most prominent acute symptoms of SCD is the painful episode known as a sickle cell crisis. These crises occur when sickle-shaped cells obstruct blood vessels, causing severe pain in the chest, abdomen, joints, and bones. The pain can be sudden and intense, requiring immediate medical attention. Additionally, individuals with SCD often suffer from anemia, a condition marked by a shortage of healthy red blood cells. This leads to fatigue, weakness, and pale skin, as the body struggles to deliver adequate oxygen to tissues.
Swelling in the hands and feet, known as dactylitis, is another common acute symptom. This condition results from blocked blood flow, causing painful swelling and inflammation. Frequent infections are also prevalent among individuals with SCD, as the spleen—an organ critical for fighting infection—can become damaged or non-functional due to the repeated blockage of blood flow, making the body more susceptible to bacterial infections.
Chronic complications of sickle cell disease can be severe and impact multiple organ systems. For instance, the spleen, liver, kidneys, and heart can all incur lasting damage from the continuous obstruction of blood flow. This can lead to conditions such as splenic sequestration, chronic kidney disease, and cardiomegaly. Children with SCD often experience delayed growth and puberty due to the body's ongoing struggle to meet oxygen and nutrient demands. The persistent blockage of blood vessels can also result in chronic pain and leg ulcers, further complicating the lives of those affected.
The underlying cause of these symptoms and complications is the sickle-shaped red blood cells. These cells are rigid and sticky, causing them to clump together and block blood flow in small blood vessels. This blockage prevents oxygen from reaching tissues, leading to pain and organ damage. Understanding these manifestations is crucial for managing and treating sickle cell disease effectively.
Treatment Options and Management Strategies for Sickle Cell Disease
Effective management of sickle cell disease (SCD) encompasses a range of treatment options and strategies aimed at alleviating symptoms, preventing complications, and improving overall quality of life. One of the primary treatment methods is the use of medications, with hydroxyurea being a cornerstone in SCD management. Hydroxyurea has been shown to significantly reduce the frequency of pain crises and acute chest syndrome, thereby improving the patient's quality of life. It works by increasing the production of fetal hemoglobin, which helps prevent the formation of sickle-shaped red blood cells.
Blood transfusions are another critical intervention, particularly for managing severe anemia and preventing stroke in children with SCD. Regular blood transfusions can help maintain adequate hemoglobin levels and reduce the risk of complications. However, long-term transfusion therapy requires careful monitoring to prevent iron overload and alloimmunization.
A bone marrow transplant, also known as a stem cell transplant, offers the only potential cure for SCD. This procedure involves replacing the patient's bone marrow with healthy marrow from a compatible donor. While bone marrow transplants have shown success in curing SCD, they are not suitable for all patients due to the risks involved and the difficulty in finding a matched donor. Therefore, this option is typically reserved for severe cases with a suitable donor.
Preventive care plays a crucial role in managing SCD. Vaccinations against infections such as pneumococcus, meningococcus, and Haemophilus influenzae type B are vital, given the increased susceptibility of SCD patients to infections. Regular health check-ups and screenings are also essential to monitor the disease's progression and manage any complications early.
Lifestyle modifications can significantly impact the management of SCD. Patients are advised to maintain adequate hydration, avoid extreme temperatures, and engage in regular physical activity tailored to their capabilities. These measures can help reduce the frequency of pain episodes and improve overall health.
Emerging treatments and ongoing research continue to offer hope for SCD patients. Gene therapy, for example, is a promising area of research that aims to correct the genetic defect causing SCD. Clinical trials are underway to evaluate the safety and efficacy of these novel treatments. Additionally, support networks and resources are invaluable for patients and their families, offering education, counseling, and community connections to navigate the challenges of living with SCD.
