Understanding Sperm Futility Calculation
Discover the importance of sperm futility calculation in identifying reproductive faults. Learn how sperm analysis can help diagnose issues and improve fertility outcomes for couples trying to conceive.
Introduction to Sperm Futility Calculation
Sperm futility calculation is a critical component in assessing male reproductive health, particularly in the context of infertility evaluations. It serves as a diagnostic tool that helps healthcare professionals ascertain the viability and motility of sperm, both essential factors for successful fertilization. Understanding sperm quality is imperative for couples facing challenges in conception, as it provides insights into potential reproductive faults that may hinder fertility.
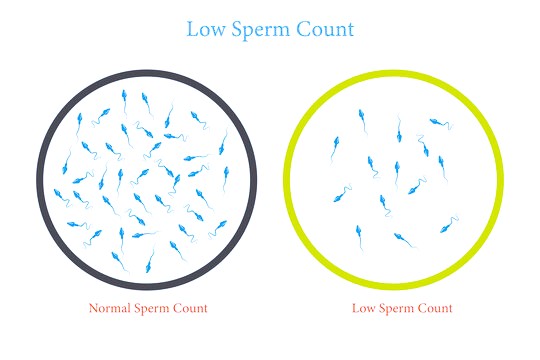
Several key parameters are involved in sperm futility calculation. These include sperm count, motility percentage, and morphology. Sperm count refers to the concentration of sperm present in a sample, while motility indicates the percentage of sperm that are actively moving. Additionally, sperm morphology assesses the shape and structure of sperm cells, which plays a vital role in their ability to fertilize an egg. A thorough evaluation of these factors allows clinicians to evaluate sperm functionality and compatibility with reproductive processes.
The significance of understanding sperm quality extends beyond mere statistics; it has profound implications for treatment decisions and reproductive outcomes. For instance, abnormalities in sperm parameters may necessitate specialized interventions or assisted reproductive technologies, such as in vitro fertilization (IVF). Therefore, accurately determining sperm futility is not only essential for diagnosis but also for creating tailored treatment plans that address specific reproductive issues.
In this context, sperm futility calculation operates as an essential framework for diagnosing and managing infertility. By carefully analyzing the various metrics associated with sperm health, medical professionals can identify underlying reproductive faults and take appropriate measures to improve the chances of conception. Thus, an in-depth understanding of sperm quality is crucial for couples navigating the complex landscape of infertility treatment.
Factors Contributing to Sperm Quality
The quality of sperm is influenced by a myriad of factors that can significantly affect sperm production, motility, and overall viability. To comprehend how sperm health can be optimized, it is vital to examine both biological and environmental influences.
Biological factors play a pivotal role in determining sperm quality. Genetics is one of the primary contributors; hereditary traits can dictate an individual’s reproductive health. Conditions such as Y chromosome microdeletions can lead to low sperm counts or infertility. Furthermore, age is a critical biological factor as sperm quality typically declines with advancing years. Men over the age of 40 may experience decreased testosterone levels, leading to diminished sperm motility and functionality.
Hormonal levels also critically influence sperm production. Testosterone, the primary male sex hormone, is essential for the development of sperm. An imbalance in hormone levels, such as low testosterone due to various health conditions, can adversely impact sperm count and quality.
Beyond biological aspects, environmental influences have a notable impact on sperm health. Lifestyle choices, including diet, exercise, and habits such as smoking or excessive alcohol consumption, can significantly affect sperm production. A diet rich in antioxidants, whole foods, and essential nutrients is associated with improved sperm motility. Additionally, exposure to environmental toxins, such as heavy metals and endocrine disruptors, can compromise sperm viability. Occupational exposures in certain industries may also elevate risks of reduced sperm quality.
Overall health is another critical factor; chronic illnesses or obesity can adversely affect hormonal balance and blood flow, leading to negative outcomes for sperm quality. By addressing these biological and environmental components, individuals can enhance their reproductive health and increase the likelihood of successful conception. Understanding and mitigating these factors are essential steps in addressing potential reproductive faults.
Assessing Female Factors in Reproductive Health
Infertility is a multifaceted issue that does not solely pertain to male factors; a significant number of cases can be traced back to female reproductive health. Understanding the female side of infertility is vital in forming a complete picture when addressing reproductive challenges. Numerous factors can contribute to female infertility, most notably ovulation disorders, which include conditions such as polycystic ovary syndrome (PCOS), hypothalamic amenorrhea, and premature ovarian insufficiency. Each of these disorders can disrupt proper ovulation cycles and diminish the likelihood of conception.
Another critical element in evaluating female fertility is the patency of the fallopian tubes. Blockages in these tubes can prevent the sperm from reaching the egg or impede the fertilized egg from traveling to the uterus. Common causes of such blockages include pelvic inflammatory disease (PID), endometriosis, and previous surgeries, which may have inadvertently caused scarring or adhesions. Therefore, assessing the condition and function of the fallopian tubes is imperative for a thorough understanding of reproductive potential.
Additionally, uterine abnormalities can significantly impact fertility. Structural issues such as fibroids, polyps, or congenital malformations may interfere with implantation or growth of a fertilized egg. Hormonal imbalances also play a critical role in female fertility, as hormones must be finely balanced to maintain regular menstrual cycles and support early pregnancy viability. Factors such as stress, lifestyle choices, and age further complicate the scenario, often aggravating existing conditions.
When assessing infertility, it is essential to adopt a comprehensive approach that considers the interplay between female factors and male sperm quality assessments. Identifying reproductive faults involves evaluating both partners, as the successful conception and maintenance of a pregnancy rely on the intricate interactions between male and female reproductive systems. Only by recognizing these multifactorial influences can effective solutions be identified and tailored for couples seeking to enhance their fertility outcomes.
Identifying the Source of Fertility Issues
Understanding the underlying causes of infertility is crucial for couples trying to conceive. Infertility can stem from various factors, and it is essential to determine whether these issues originate from the male or female partner. The identification of the source involves a series of scientific evaluations and tests designed to uncover potential reproductive faults.
For men, a semen analysis serves as a foundational test in assessing male fertility. This analysis examines several important parameters, including sperm count, motility, and morphology. Sperm motility refers to the movement and vitality of the sperm, while morphology considers the size and shape of sperm cells. An abnormal result in any of these areas may indicate male factor infertility, prompting targeted treatments or further investigations, such as hormonal assessments to evaluate endocrine function.
For women, the evaluation of hormonal health is pivotal. Hormonal evaluations include measuring levels of key reproductive hormones, such as luteinizing hormone (LH), follicle-stimulating hormone (FSH), and estradiol, among others. These tests help to ascertain whether ovulation occurs regularly and if any hormonal imbalances might hinder fertility. Additionally, imaging tests such as ultrasound can provide insight into the physical status of reproductive organs, helping to identify conditions like polycystic ovary syndrome (PCOS) or uterine abnormalities that contribute to infertility.
Recent advancements in reproductive technology have further refined the process of diagnosing infertility. Techniques such as advanced sperm function tests, genetic testing, and laparoscopy bring us closer to identifying precise causes. By employing these cutting-edge approaches, healthcare professionals can formulate tailored treatment plans designed to address the specific needs of couples facing fertility challenges. Understanding whether the infertility issue lies with the male or female partner is a significant step toward effective resolution and successful conception.
