Understanding Sperm: Production, Lifecycle, and Key Details
Learn all about understanding sperm, including the production process, lifecycle, and key details. Explore the fascinating world of sperm and how it plays a crucial role in reproduction.
What is Sperm?
Sperm, or spermatozoa, are the male reproductive cells essential for sexual reproduction. Produced in the testes, these cells play a pivotal role in fertilization by combining with the female egg, or ovum, to form a zygote, thus forming the foundation for creating new life. Understanding sperm's structure and function provides insight into their critical role in human reproduction.
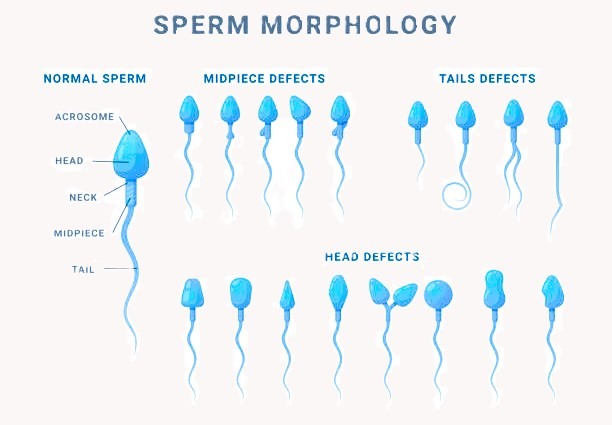
Structurally, sperm cells are unique and highly specialized. Each sperm consists of three main parts: the head, midpiece, and tail. The head houses the nucleus, which contains 23 chromosomes—half the genetic material required for human development. This nucleus is capped by the acrosome, an enzyme-filled sac that aids in penetrating the egg during fertilization. The midpiece is packed with mitochondria, the powerhouse of the cell, providing the energy necessary for the sperm's movement. The tail, or flagellum, propels the sperm towards the egg with a whip-like motion, a crucial feature for successful fertilization.
The motility of sperm—its ability to move—is a defining characteristic, driven by the tail and the energy from the midpiece. This motility is essential, as sperm must traverse the female reproductive tract to reach and penetrate the egg. Without adequate motility, the chances of successful fertilization diminish significantly. Additionally, the sperm's genetic material plays a fundamental role in passing on genetic information to the offspring, ensuring the continuity of genetic traits from generation to generation.
In essence, sperm are not merely carriers of genetic information but are actively involved in the complex process of fertilization. Through their unique structure and specialized functions, sperm ensure the delivery of paternal DNA to the ovum, enabling the development of a viable embryo. This remarkable process underscores the vital contribution of sperm to reproduction and the perpetuation of life.
How and When is Sperm Produced?
Spermatogenesis is the intricate, multi-stage process through which sperm is produced in the male testes. This process begins with spermatogonia, the sperm precursor cells located within the seminiferous tubules. During spermatogenesis, these cells undergo a series of transformations, including mitosis and meiosis, ultimately giving rise to mature spermatozoa.
The production of sperm is initiated during puberty, marking the onset of male reproductive capability. At this stage, the hypothalamus starts secreting gonadotropin-releasing hormone (GnRH), which signals the pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH). In response to LH, the Leydig cells in the testes produce testosterone, a crucial hormone for spermatogenesis. Concurrently, FSH acts on the Sertoli cells, facilitating the nourishment and support of developing sperm cells.
The timeline of sperm development involves several key stages: spermatogonia first undergo mitotic division to increase their number. Subsequently, these cells enter meiosis I, transforming into primary spermatocytes, followed by meiosis II, resulting in secondary spermatocytes. The final stage involves the differentiation of these cells into spermatids and then into fully mature spermatozoa through a process called spermiogenesis. This entire process takes approximately 64 days.
Various factors can influence sperm production, including age, health, and lifestyle choices. As men age, the efficiency of spermatogenesis may decline, leading to reduced sperm counts and motility. Health conditions, such as infections, hormonal imbalances, and certain genetic disorders, can also adversely impact sperm production. Lifestyle habits, including diet, exercise, smoking, and alcohol consumption, play a significant role in maintaining optimal sperm health.
Understanding the complexities of spermatogenesis underscores the importance of maintaining a healthy lifestyle and monitoring factors that could affect reproductive health. The coordinated interplay of hormones and cellular processes in the testes is essential for the continuous production of viable sperm, which is crucial for male fertility and overall reproductive success.
Factors Affecting Sperm Quality and Quantity
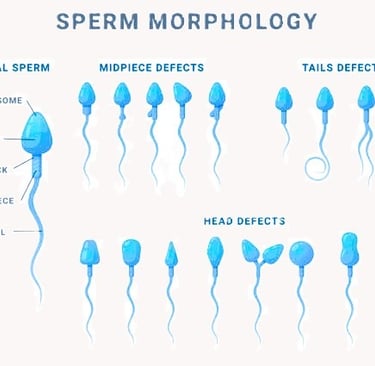
Sperm quality and quantity are influenced by a wide array of both internal and external factors. Genetic predispositions play a significant role in determining baseline sperm parameters, including count, morphology, and motility. Beyond genetics, environmental factors profoundly impact sperm health. Exposure to toxins, such as pesticides and heavy metals, has been linked to decreased sperm count and impaired functionality. Additionally, lifestyle choices such as diet, exercise, and stress levels can either enhance or deteriorate sperm quality.
Dietary habits are particularly important; a diet rich in antioxidants, vitamins, and minerals supports optimal sperm production. Omega-3 fatty acids, zinc, and folate, found in foods like fish, nuts, and leafy greens, are specifically vital for maintaining healthy sperm. Conversely, excessive consumption of processed foods, alcohol, and caffeine can negatively affect sperm parameters. Regular physical activity enhances blood circulation and hormone levels, further promoting healthy spermatogenesis. However, excessive exercise or use of anabolic steroids can yield the opposite effect, impairing sperm quality.
Stress management is another critical factor. Chronic stress elevates cortisol levels, which may inhibit testosterone production, leading to reduced sperm count and motility. Mindfulness practices, adequate sleep, and leisure activities can help mitigate stress and its adverse effects on sperm health.
Medical conditions and treatments also impact spermatogenesis. Conditions such as varicocele, infections, and hormonal imbalances can significantly impair sperm production. Varicocele, an enlargement of veins within the scrotum, can result in decreased sperm count and poor morphology. Chronic infections, including sexually transmitted infections, can lead to scarring and blockages, further hindering sperm passage. Hormonal imbalances, often stemming from conditions like hypogonadism, disrupt the complex hormonal interplay essential for sperm production.
Regular medical check-ups enable early detection and management of these issues. Adopting a healthy lifestyle, including balanced nutrition, regular exercise, and stress reduction, is paramount in maintaining and improving sperm quality and quantity. Making informed choices and seeking medical advice when necessary can significantly enhance reproductive health outcomes.
